腎癌 Renal Cancer


腎癌是甚麼?

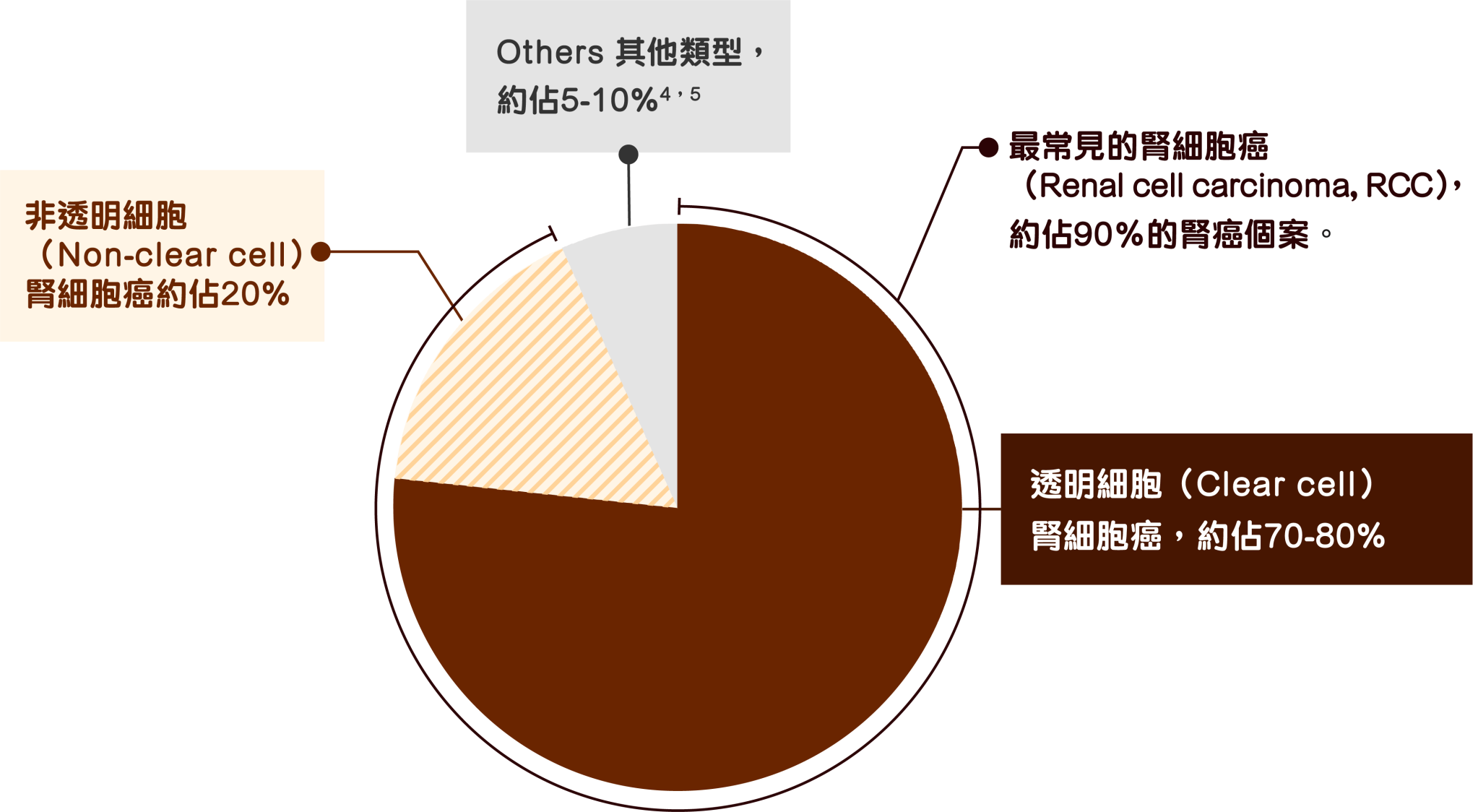
腎癌種類
腎癌可以依據細胞型態分為2,3:

腎癌統計數字
在香港,腎癌*是男性中第7常見的癌症:在2022錄得的838宗新症個案中,有562宗為男性。6,7
另外,腎癌*的呈報個案在近20年持續上升。7 不止本港,腎癌個案在全球都有增多的趨勢,估計與科技進步幫助更早檢測出早期個案,以及肥胖和高血壓患者增多等有關。8,9,10
*腎及其他泌尿器官(膀胱除外)的癌症

腎癌的成因
醫學界尚未能完全破解腎癌的成因,但有些因素可能增加患上腎癌的機會,包括11,12:
- 男性
- 年紀較大(如65歲或以上)
- 長期吸煙
- 過重
- 高血壓
- 家族病史
- 遺傳:例如希佩爾-林道綜合症(Von Hippel-Lindau disease, VHL)、結節性硬化症等會增加患腎癌的風險
- 長期腎病,如慢性腎衰竭或長期洗腎者
- 長期於工作環境接觸重金屬、三氯乙烯等化學物
- 長期服用某些止痛藥
腎癌症狀
腎癌早期可能沒有明顯徵狀,超過一半的個案均是進行身體檢查或掃描檢查中偶然發現。2
如果出現上述症狀,應盡早求醫找出病因。
腎癌分期
與其他癌症一樣,腎癌可以根據美國癌症聯合委員會(AJCC)的TNM系統分期,即腫瘤的大小及影響範圍(T),以及是否擴散到淋巴結(N)及遠端器官(M),幫助醫生評估病情的嚴重程度及預期後果。14
| 分期 | |
|---|---|
| 第1期 | 腫瘤直徑小於7厘米並局限在腎臟內,未有擴散至淋巴結或其他器官 |
| 第2期 | 腫瘤直徑大於7厘米但局限在腎臟內,尚未擴散到淋巴結或其他器官 |
| 第3期 |
|
| 第4期 |
|
診斷及生物標記檢測


腎癌治療方案

腎癌的治療取決於腫瘤分期及患者情況和需要而定。早期腎癌所需的治療較簡單。21
腎癌術後治療
手術通常是非末期腎細胞癌(最常見的腎癌)的首選治療方法。但在以手術切除腫瘤後,有大約4成患者的癌症會復發,且大部分會在3年內復發。這時候,術後治療就成爲腎癌患者治療方案中重要的一環。25
腎細胞癌的術後輔助治療是指在手術之後進行免疫治療,旨在消滅患者體內剩餘的癌細胞(尤其是肉眼看不到的),從而減低癌症復發的機會,延長患者壽命。25,26
由於腫瘤的分期、大小、分級等都會影響患者的復發風險,泌尿科醫生通常會在術後為患者進行評估,並爲有高復發風險的腎癌患者建議在手術後的12週内進行免疫治療,為期一年。詳情可向醫生查詢。25,27
對於腎癌患者而言,由多個專科(包括泌尿外科、腫瘤科及放射治療科等)醫生組成的跨專業團隊,可以因應腫瘤的分期、位置及個人健康狀況等等,制訂適切的治療方案以獲取最理想的控病效果。15,28
手術切除是腎癌最主要的治療方法,其他非手術治療則有免疫治療、消融術、化療、放射治療、及標靶治療等。1,29
現在問,發現更多可能!向醫生了解不同療法的優點和可能副作用,一起制定最適合的治療方案。
常見問題

腎細胞癌是其中一種常見的腎癌。2,3 在早期腫瘤還小(小於3厘米)時,患者通常不會有任何症狀,而是在常規放射檢查中偶然發現的。30
早期腎癌所需的治療較簡單。體積細小的第一期腎癌患者可能毋須治療,只需要定期覆診作積極監察便可;而第一至三期腎癌普遍以手術為主要治療手段,並視乎情況再配合術後治療(如免疫治療)。21
晚期腎細胞癌通常指腫瘤已經走出腎臟外層的筋膜,侵犯腎上腺,並可能已擴散到附近淋巴結,但未影響其他器官;或出現了遠端淋巴結或器官轉移。14
腎癌的跨專科醫療團隊可包括泌尿科醫生、放射科醫生、腫瘤科醫生、泌尿科臨床護士等。31
由二個或以上專科醫生/醫護人員組成的醫療團隊會一同負責患者的治療方案,確保為每個患者制定最適合的個人化治療,在治愈癌症的同時,延長患者壽命,提高生活水平。31,32
手術切除是腎癌的主要治療手術,1 僅餘一個腎臟仍足以應付身體的需要,不會對健康產生不良影響。33
腎癌患者切除一邊腎臟後,需要留意及跟進腎臟狀況,故此需要定期覆診,同時亦要盡力保護剩餘的腎臟及功能,包括33:
- 遠離煙酒
- 均衡飲食
- 恆常運動
- 控制血壓及其他病患
腎癌患者在康復後,可以恢復正常的步伐,並建議採取健康的飲食模式,有助預防復發及維持腎臟功能,包括34,35:
- 控制鹽份攝取
- 飲用足夠水份
- 控制蛋白質攝取
有研究指高蛋白飲食可能與腎癌及腎功能有關,應與醫生了解是否需要控制蛋白質攝取。


1. National Kidney Foundation. Kidney cancer. Available at: www.kidney.org/kidney-topics/kidney-cancer. Accessed Sep 2024. 2.Pandey J, Syed W. Renal cancer. Available at: www.ncbi.nlm.nih.gov/books/NBK558975/. Accessed Sep 2024. 3. American Cancer Society. What is kidney cancer? Available at: www.cancer.org/cancer/types/kidney-cancer/about/what-is-kidney-cancer.html. Accessed Sep 2024. 4. Uhlig J, et al. Renal sarcomas: Epidemiology, treatment and outcomes. Journal of Clinical Oncology 2021. 39:6. 5. NCBI. Wilms Tumor. Available at: https://www.ncbi.nlm.nih.gov/books/NBK442004/. Accessed on Apr 2025. 6. Hong Kong Cancer Registry, Hospital Authority. Leading cancer sites in Hong Kong in 2022. Available at: www3.ha.org.hk/cancereg/pdf/top10/rank_2022.pdf. Accessed Jan 2025. 7. Hong Kong Cancer Registry, Hospital Authority. Hong Kong cancer statistics: Incidence, both sex, broad age group, 2003–2022, kidney and other urinary organs except bladder, by year and age group. Available at: www3.ha.org.hk/cancereg/allages.asp. Accessed Jan 2025. 8. Jani C, et al. Sci Rep 2022;12:22368. 9.NCBI. Renal Cancer. Available at: https://www.ncbi.nlm.nih.gov/books/NBK558975/. Accessed on Apr 2025. 10. Cirllo L, et al. Global epidemiology of kidney cancer. Nephrol Dial Transplant 2024. 39:920-928. 11. American Cancer Society. Risk factors for kidney cancer. Available at: www.cancer.org/cancer/types/kidney-cancer/causes-risks-prevention/risk-factors.html. Accessed Sep 2024. 12. Cancer Research UK. Risks and causes of kidney cancer. Available at: www.cancerresearchuk.org/about-cancer/kidney-cancer/risks-causes. Accessed Sep 2024. 13. American Cancer Society. Kidney cancer signs and symptoms. Available at:www.cancer.org/cancer/types/kidney-cancer/detection-diagnosis-staging/signs-and-symptoms.html. Accessed Sep 2024. 14. American Cancer Society. Kidney cancer stages. Available at: www.cancer.org/cancer/types/kidney-cancer/detection-diagnosis-staging/staging.html. Accessed Sep 2024. 15. Cancer Research UK. Tests for kidney cancer. Available at: www.cancerresearchuk.org/about-cancer/kidney-cancer/getting-diagnosed/tests-for-kidney-cancer. Accessed Sep 2024. 16. American Cancer Society. Tests for kidney cancer. Available at: www.cancer.org/cancer/types/kidney-cancer/detection-diagnosis-staging/how-diagnosed.html. Accessed Sep 2024. 17. NHS. Tests and next steps for kidney cancer. Available at: www.nhs.uk/conditions/kidney-cancer/tests-and-next-steps/. Accessed Sep 2024. 18. National Cancer Institute. Renal cell cancer treatment (PDQ®) – Patient version. Available at: www.cancer.gov/types/kidney/patient/kidney-treatment-pdq. Accessed Sep 2024.19. National Cancer Institute. Biomarker testing for cancer treatment. Available at: www.cancer.gov/about-cancer/treatment/types/biomarker-testing-cancer-treatment. Accessed Jan 2025. 20. Saliby RM, et al. Am Soc Clin Oncol Educ Book 2024;44:e430734. 21. American Cancer Society. Treatment of kidney cancer by stage. Available at: www.cancer.org/cancer/types/kidney-cancer/treating/by-stage.html. Accessed Sep 2024. 22. NCCN. NCCN Clinical Practice Guidelines in Oncology: Kidney cancer (version 2.2025 – September 6, 2024). Available at: 23. Martini A, et al. Neoadjuvant and adjuvant immunotherapy in renal cell carcinoma. World Journal of Urology 2021. 39(5):1369-1376. 24. Janowitz T, et al. Adjuvant Therapy in Renal Cell Carcinoma—Past, Present, and Future. Semin Oncol 2013. 40(4):482-91. 25. Cosso F, et al. Int J Mol Sci 2023;24:4243. 26. West H, Jin J. JAMA Oncol 2015;1:698. 27. Lalani AA, et al. Can Urol Assoc J 2023;17:E154-E163. 28. American Cancer Society. Health professionals who are part of a cancer care team. Available at: www.cancer.org/cancer/managing-cancer/finding-care/health-professionals-associated-with-cancer-care.html. Accessed Sep 2024. 29. Powles T, et al. Ann Oncol 2024;35:692-706. www.nccn.org/professionals/physician_gls/pdf/kidney.pdf. Accessed Sep 2024. 30. Garfield K, LaGrange CA. Renal cell cancer. Available at: www.ncbi.nlm.nih.gov/books/NBK470336/. Accessed Sep 2024. 31. Macmillan Cancer Support. Multidisciplinary team (MDT) for kidney cancer. Available at: www.macmillan.org.uk/cancer-information-and-support/kidney-cancer/mdt. Accessed Sep 2024. 32. Zeng Y, et al. J Multidiscip Healthc 2023;16:503-513. 33. Cancer Research UK. Life after surgery for kidney cancer. Available at: www.cancerresearchuk.org/about-cancer/kidney-cancer/living-with/daily-life. Accessed Sep 2024. 34. Kidney Cancer Association. Life with kidney cancer. Available at: www.kidneycancer.org/patients/living-with-kidney-cancer/. Accessed Sep 2024. 35. Macmillan Cancer Support. Recovery from treatment for kidney cancer. Available at: www.macmillan.org.uk/cancer-information-and-support/kidney-cancer/recovery-from-treatment-for-kidney-cancer. Accessed Sep 2024.